Perdarahan waktu bersalin mengancam nyawa ibu
Hemorrhage is not something that we want to think about when it comes to giving birth. In fact, 95% of births will not have a problem with hemorrhage. However it is important to know the risk factors for hemorrhage and discuss your personal risk factors with your doctor or midwife.
Postpartum hemorrhage is defined as a loss of blood in the postpartum period of more than 500 mL. The average, spontaneous vaginal birth will typically have a 500 mL blood loss. In cesarean births the average blood loss rises to 800-1000 mL. There is a greater risk of hemorrhage in the first 24 hours after the birth, called primary postpartum hemorrhage. A secondary hemorrhage occurs after the first 24 hours of birth.
There are certain risk factors that make a postpartum hemorrhage more likely to happen:
- Multiple Gestation
- Large baby
- Polyhydramnios
- Multipartity (particularly grand multiparity, more than 5 term pregnancies)
- Prolonged labor (uterine inertia)
- Labor augmented with Pitocin
- General Anesthesia
- Placenta Previa
- Abruptio Placentae
- Magnesium Sulfate infusion
If hemorrhage does occur there are several steps which can be taken to treat the bleeding, steps used depend on the reason for the bleeding:
- Uterine massage
- Have the mother in the trendelenberg position (Feet above heart)
- Give oxygen
- Ensure two large IV sites are available
- Give Medications (Several types: Pitocin, methergine, hemabate)
- Consider surgery including ligation of Uterine and Hypogastric arteries and/or hysterectomy (removal of the uterus)
Some hospitals and birth centers choose to give every woman a routine injection of pitocin to help prevent hemorrhage and to help ensure that the placenta comes quickly and easily. However, many choose a more natural route, which is to wait and see if there is a bleeding problem. Many also encourage the American Academy of Pediatrics recommendation of breastfeeding beginning as soon as possible after birth. This allows the mother to secrete her own oxytocin to help contract the uterus and expel the placenta.
Massaging the uterus is also done to help expel clots of blood. It is also used to check the tone of the uterus and ensure that it is clamping down to prevent excessive bleeding. Poor tone of the uterus at this point is what causes 70% of the cases of postpartum hemorrhage. This can be uncomfortable to painful. Be sure to utilize any and all relaxation and breathing techniques and not tense your abdominal muscles. If it is too painful, medications can also be used. This will be done with decreasing frequency after the birth, as your bleeding slows.
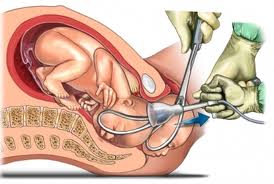
Ensuring your bladder is empty will also help you avoid hemorrhage. Simply emptying the bladder in any manner can do this. Women who have not used regional anesthesia can usually use the restroom themselves within the hour after birth. Those who had regional anesthesia can use the restroom or bedpan in varying time increments, but usually within an hour of the anesthesia wearing off, unless a cesarean was performed. Catheterization can also be of benefit here, including both the indwelling catheter (usually done for cesareans and those with major urethral trauma) or what is called an "in/out" or "straight cath" to drain the urine and allow the bladder to not impede the uterus.
Talking to your practitioner to see which after birth protocol he or she uses and what might be best for your situation can go a long way in helping you to understand your personal risk factors and prevention strategy for postpartum hemorrhage.











{ 0 komentar... Views All / Send Comment! }
Posting Komentar